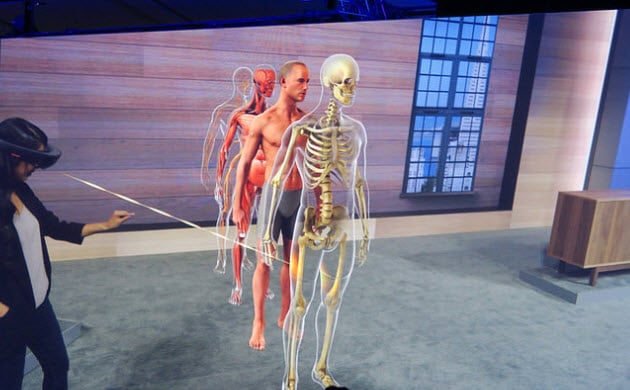
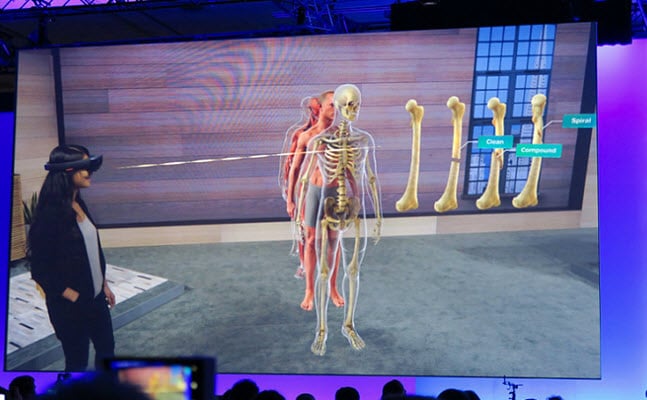
Imagine being a patient in a hospital bed, and you slip on a headset that visually illustrates your current and historical health status allowing you to track your progress towards recovery. If you’re a medical student, imagine being able to sit in an empty classroom on campus, put on a headset, and be able to examine a realistic computer generated model of the human body to further your understanding of anatomy. As far-fetched as these scenarios may seem, they are closer to reality than you might think.
The technologies that will make these scenarios possible are virtual reality (VR) and augmented reality (AR). While the terms are often used interchangeably they are two different technologies:
- VR: A computer-generated simulation that produces sight, sound, and touch stimuli so that individuals experience a completely separate environment.
- AR: Produces computer-simulated stimuli that are added to the individual’s current space so that the individual’s experience of their current environment is altered.
Currently engineers, physicians, other healthcare providers, and educators are working to create innovative ways to apply these immersive technologies in order to transform clinical teaching and practice. Research suggests that VR and AR will take on a larger role in the next few years. According to a recent ABI Research study, VR services in the healthcare market generated around $9 million in 2017 and this is forecasted to grow to approximately $285 million by 2022.1
Medical student education and resident training, patient therapy, and physician operations are three segments in healthcare with high growth potential for VR and AR technologies.
1. Medical Student and Resident Training
I may be biased since I recently completed my medical school training, but one of the most exciting focuses of virtual reality is medical education. A recently published article in the Journal of the American Medical Association (JAMA) illustrates that Dr. Albert “Skip” Rizzo, Director of Medical Virtual Reality at the Institute of Creative Technologies at the University of Southern California, is using artificial intelligence and virtual reality to develop patient simulations complete with personalities and accurate clinical circumstances.2 These virtual patients have been used to train students in how to demonstrate empathy and practice having tough talks about substance abuse, mental illness, and sexual assault.
Several American medical and nursing schools like Stanford, Texas Tech, and San Diego State University have already incorporated AR and VR technologies, like HoloPatient, into their medical education curriculums.
- HoloPatient, the result of a partnership between Pearson and Microsoft HoloLens, provides students with a realistic 3D hologram of a patient who exhibits a variety of symptoms and behaviours which need to be examined and diagnosed.
- Dr. David Axelrod, an Assistant Professor of Pediatrics at Stanford University School of Medicine, is developing a new VR curriculum called Stanford Virtual Heart.3 This was developed to provide better insights into how the heart operates and what happens when something goes wrong.
- At Case Western Reserve University School of Medicine students are able to use an app called Holo Anatomy in which they can virtually dissect a human body in order to better understand important structures and organ systems.
2. Physician Work Streams
Other AR and VR technologies are geared to easing the administrative workload, a common cause of burnout amongst physicians, and in doing so allow them to spend more time providing direct patient care. The most recent example of this kind of AR application is Augmedix, which uses Google glasses to allow for remote scribing of patient notes in real time.
By streamlining administrative work, AR and VR technologies could allow hospitals and private physician groups to increase their revenues by seeing more patients each day. While this is a clear benefit, it is important to consider other factors such as the cost of the technology, privacy risks for patients’ medical information, and whether groups can get buy-in from providers and patients that will allow them to use this innovative technology effectively.
3. Patient Care and Outcomes
The main focus of any change to healthcare is to improve patient outcomes. Augmented or virtual reality can enhance a patient’s perception of their surroundings and can be beneficial when treating a variety of illnesses especially those that require cognitive behavioral therapy (CBT). So far these technologies have seen the most impact in assisting patients going through physical therapy, helping with pain management, and in addressing their fears, phobias, and anxiety.
Scientific evidence suggests that VR and AR have the ability to relieve pain in both the short and in some cases long term.4 Neurologic and psychologic exams have shown that the somatosensory cortex, the part of the brain that perceives pain, shows decreased activation when a patient is engaging in VR. VR therapy is also helping amputee patients deal with pain associated with their “phantom limbs”. Patients put on a VR headset and then undergo a process called “virtual mirror” therapy in which they are able to control a virtual version of their absent limb. Treating amputee patients has traditionally been very difficult because the pain often doesn’t respond to opioids and other pain relievers.
If you’re a patient recovering from trauma and undergoing physical therapy, would you rather go to a therapist and do a variety of weight resistance routines? Or, would you rather employ AR/VR to track your body movements and allow your therapy to occur within a virtual game? Doing exercises in virtual reality is likely to be more fun, less hassel (and easier to gamify) compared with doing them in a gym, so people will be more likely to exercise.
For those patients who have a range of fears, phobias, and anxieties ranging from a fear of heights, spiders, or flying on the low end to something as severe as post-traumatic stress disorder (PTSD), VR/AR technologies might be the perfect solution. Most psychiatrists will treat specific phobias through a process called exposure therapy in which patients are slowly introduced to their fears. VR is ideal for these patients because the provider can adjust the settings based on the needs of each patient and the amount of exposure they need.
Conclusion
VR and AR technologies should not replace the tried and true processes of learning (books, cadavers, time in the hospital) and practicing medicine. However, these new tools can assist in maximizing the quality of learning, efficiency of workstreams, and proficiency of patient care.
Kevin Anderson is a graduating medical student at Duke University School of Medicine and will be starting at LEK Consulting later this year. He’s most passionate about healthcare redesign, patient engagement, and the life sciences. His free moments are spent traveling and enjoying sporting events with his wife and daughter.
References:
- “Virtual Reality in Medicine and Healthcare to Generate US$285 Million in 2022.” ABI Research, 5 Oct. 2017, abiresearch.com/press/virtual-reality-medicine-and-healthcare-generate-u/.
- Kuehn, Bridget M. “Virtual and Augmented Reality Put a Twist on Medical Education.” JAMA, vol. 319, no. 8, 2018, p. 756., doi:10.1001/jama.2017.20800
- “The Stanford Virtual Heart – Stanford Children’s Health.” Stanford Children’s Health – Lucile Packard Children’s Hospital Stanford, stanfordchildrens.org/en/innovation/virtual-reality/stanford-virtual-heart.
- Li, Angela, et al. “Virtual Reality and Pain Management: Current Trends and Future Directions.” Pain Management, vol. 1, no. 2, 2011, pp. 147–157., doi:10.2217/pmt.10.15.